Cocaine is a highly addictive drug – some people are unable to walk away from it after just one use. And once addicted, users can lose control of their lives. Powerful cravings, caused by the drug's ability to hijack healthy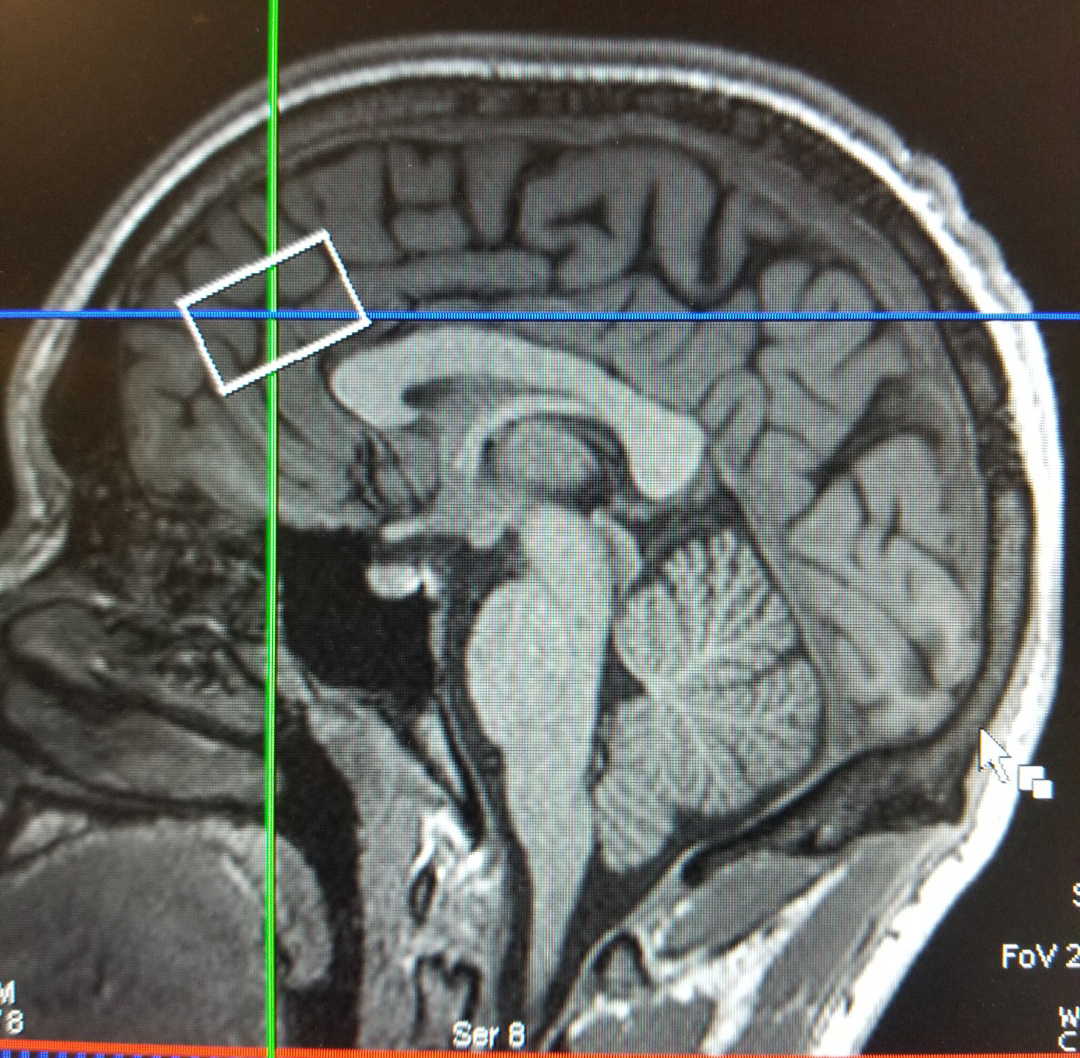 brain circuits, drive users to seek out the drug at the expense of work, friends, and family. To break free from these cravings, healthy brain function and behaviors must be reestablished. Existing treatments attempt to do this, but they often fail to produce long-lasting recovery.
brain circuits, drive users to seek out the drug at the expense of work, friends, and family. To break free from these cravings, healthy brain function and behaviors must be reestablished. Existing treatments attempt to do this, but they often fail to produce long-lasting recovery.
Researchers at the Lewis Katz School of Medicine at Temple University (LKSOM) hope to soon change that, thanks to a new $1.77M grant from the National Institute on Drug Abuse (NIDA) that will allow them to explore whether a drug called clavulanic acid can help patients recover from cocaine use disorder. Clavulanic acid is part of an existing therapy known as Augmentin. Augmentin combines clavulanic acid with the penicillin-related antibiotic amoxicillin and is used for the treatment of bacterial infections.
“Augmentin has been around since the 1980s, but interest in the clavulanic acid component as a form of treatment for drug addiction is recent,” explained Mary Morrison, MD, MS, Vice Chair for Research, Psychiatry and Professor of Psychiatry and Behavioral Science at LKSOM, and senior investigator on the new grant.
The idea that clavulanic acid could serve as a therapy for drug addiction emerged in 2014, from work carried out in the laboratory of Scott Rawls, PhD, Professor of Pharmacology at the Center for Substance Abuse Research at LKSOM. Dr. Rawls is a co-investigator on the new NIDA grant.
“Much of the research in my laboratory centers on an excitatory signaling molecule in the brain called glutamate, transmission of which is significantly altered by cocaine use,” Dr. Rawls said. “Our research has shown that increased glutamate transmission in the brain is associated with addictive-like behaviors.” Drugs that normalize glutamate transmission are thought to be critical to reducing cocaine craving and vulnerability to cocaine relapse.
Clavulanic acid is a promising drug in this regard. In preclinical studies in animals carried out by Dr. Rawls and colleagues, clavulanic acid was found to enhance glutamate uptake in brain cells called astrocytes. It did so by increasing the expression of a specialized glutamate transport molecule known as glutamate transporter subtype 1 (GLT-1). Dr. Rawls's laboratory further showed in animals that clavulanic acid reduces cocaine-induced activation of biological reinforcement and motivational systems – the biological reward pathways that keep cocaine users engaged in drug-seeking behavior.
The preclinical data, by providing evidence that clavulanic acid might be repurposed to treat cocaine use disorder, laid the basis for the clinical study in human patients that will be funded by the new NIDA award. The clinical study will involve the use of functional magnetic resonance imaging (fMRI) to examine the brain in persons with recent cocaine addiction. “Spectroscopy will allow us to observe changes in glutamate levels in the brain, and adding fMRI will enable us to look at associated changes in cocaine craving,” Dr. Morrison said.
The NIDA award provides support for Dr. Morrison's clinical study of clavulanic acid for one year. If the drug is found to reduce cocaine craving and is safe and well-tolerated in hospitalized patients, the research team will receive additional funding to pursue an outpatient treatment study. This second phase of the study, in which cocaine users would take clavulanic acid outside a hospital setting, would involve patients across multiple U.S. cities.
Other co-investigators on the award include fellow Department of Psychiatry, Center for Substance Abuse Research, and Lewis Katz School of Medicine colleagues Dr. Helene Khalid, NIDA Postdoctoral Fellow in Psychiatry; Dr. M. Ingre Walters, Associate Professor in Clinical Psychiatry and Behavioral Sciences; Dr. Daohai Yu, Professor of Clinical Sciences; and Dr. Huiling Peng, Neuroimaging Supervisor. Collaborators from the University of Pennsylvania and Harvard University will provide neuroimaging consultation.
Photo caption: This is an image of the sagittal slice of the brain looking specifically at the anterior cingulate cortex (ACC). The white box is representing the coverage of the ACC.
