 How do you study something complex like HIV-associated neurocognitive disorders (HAND) when you can’t collect the one thing that is critical to the research – live brain tissue?
How do you study something complex like HIV-associated neurocognitive disorders (HAND) when you can’t collect the one thing that is critical to the research – live brain tissue?
If you’re a scientist, you create a model.
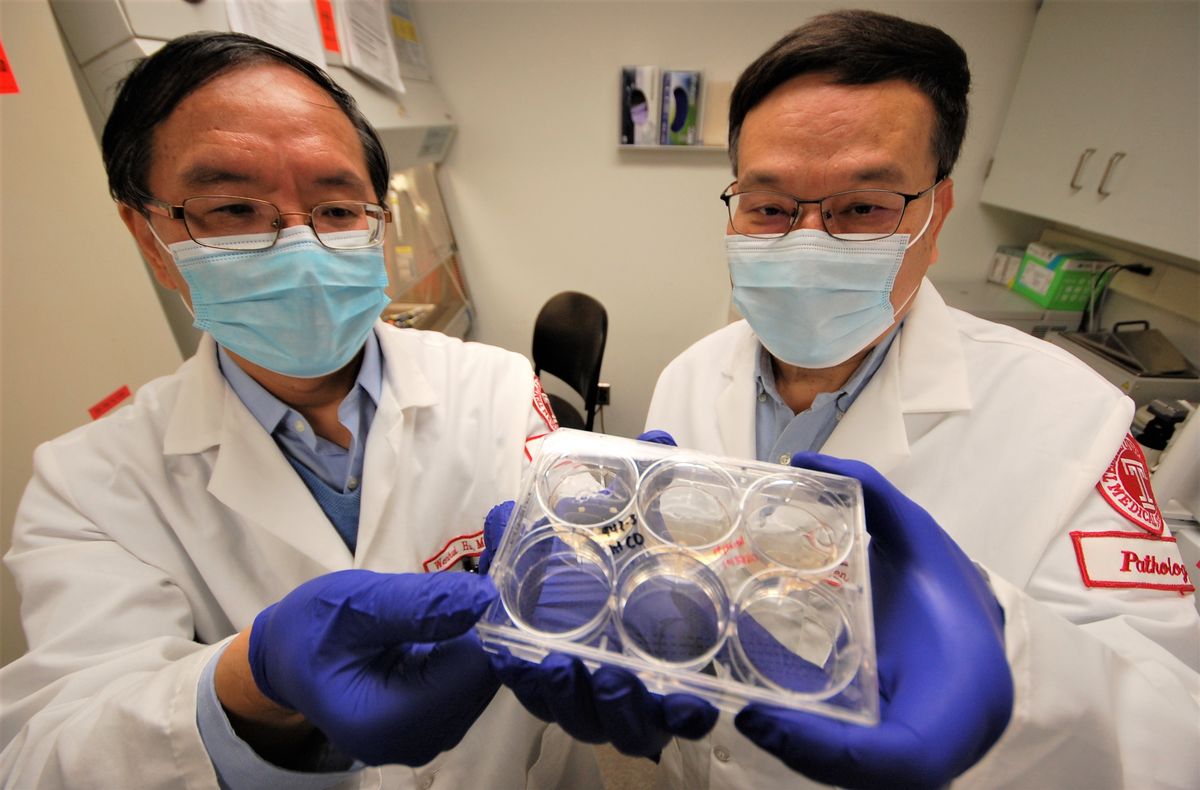
Recently, two researchers from the Lewis Katz School of Medicine received a $3.4 million grant from the National Institutes of Health to generate human brain organoids, or “mini-brains,” on which they will study the impact of HIV infection and methamphetamine (meth) on the central nervous system.
Mini-brains are 3D tissue structures generated from pluripotent stem cells in a test tube. The mini-brains contain different cell types and represent the anatomical structure of an actual brain.
“These mini-brains provide physiologically relevant tissue for the study of HAND, something which has been hampered in the past by difficulties in collecting and culturing live brain tissues,” says Wenzhe Ho, MD, MPH, a Professor in the Department of Pathology and Laboratory Medicine and in the Center for Substance Abuse at Temple.
“Unlike mini-brain models developed by other investigators, we will generate one that not only contains the ordinary brain cells, but also the resident immune cells – called microglia – which are the cells HIV targets. Our mini-brain model is called ’microgliacontaining cerebral organoid,‘ or MCO for short.”
Meth is a powerful, highly addictive stimulant that affects the central nervous system. It is one of the most abused drugs in America and is commonly used by HIV-infected individuals. Because both HIV and meth negatively affect the central nervous system, it’s important to understand the role the interaction of these two factors plays in the development of HAND.
Dr. Ho’s collaborator on this project is Wenhui Hu, MD, PhD, an Associate Professor in the Department of Pathology and Laboratory Medicine and in LKSOM’s Center for Metabolic Disease Research. Together, they will generate and validate the MCO model in the study of HIV infection of the brain in the context of interaction with meth.
If successful, their MCO model will allow for further research to understand the mechanism of HIV persistence in the brain, the impact of HIV and/or meth on the different types of brain cells, and the factors underlying the development of neurocognitive deficits associated with HIV infection and treatment.
“Our studies will be the first attempt to determine HIV-infected cell types and primary reservoir/latent cells in live, brain-like tissue,” Dr. Hu says. “Also, we will study how HIV and/or meth impair neural development and neuronal circuitry. Successful completion of this project should provide a clinically relevant in vitro brain model to study the roles of HIV infection and drugs of abuse in the pathogenesis of NeuroAIDS.”
